Background
The diagnosis of pancreatic ductal adenocarcinoma (PDAC) comes along with a bleak prognosis with a maximum 5-year overall survival (OS) rate of only 12% across all stages. The absence of effective prevention and screening methods, coupled with a rising incidence, has resulted in an alarming rise in the number of pancreatic cancer-related deaths, and this trend is projected to continue, positioning PDAC as one of the leading causes of cancer-related fatalities globally.
It is an established standard to discuss diagnosis and treatment options for each patient in a multi-disciplinary tumor board (MDTB). However, not only due to the number of patients
and various specialist being involved, but also due to individually tailored treatment concepts rather than a rigid and universally applicable standard, the exact number of patients ending up in each group of treatment options (upfront-surgery, neoadjuvant chemotherapy, palliative concepts, best-supportive care) remains unknown, especially if not a cross-section at time “X” but a longitudinal section over time “Y” is considered.
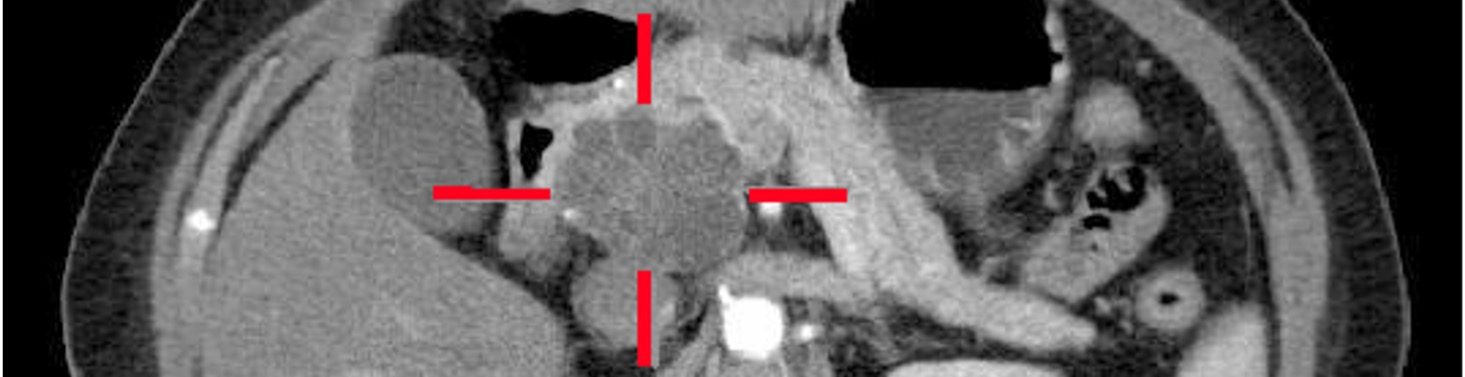
The aim of the current study is to exactly quantify the number of patients categorized by National Comprehensive Cancer Network (NCCN)-criteria in (upfront-)resectable (R), borderline resectable (BR) and locally advanced (LA) by the time of primary diagnosis, and, more important, over a follow-up period of nine months, objectify the management of each group.
Design
Global evaluation of the management of PDAC patients by resectability as decided at MDTB, designed as an international prospective snapshot study. Each center will recruit patients in their MDTB over three months. Secondly, patients will be followed for 9 months, covering information about their individually tailored treatment, including chemotherapy-protocols, therapy switch, surgery or surgery after neoadjuvant therapy, side-effects from therapy and switches to resectability and palliative treatment including reasons for it. Find a short overlook here (Flyer)